Why Am I So Tired? The Hidden Link Between Aging and Nervous System Dysregulation
As we age, many of us begin to feel more tired, less resilient to stress, and generally less vibrant than we once did. These changes are often dismissed as an inevitable part of aging, but there’s a deeper, scientific explanation behind them. A key player in this process is the mitochondria—tiny structures within our cells that produce energy and regulate various cellular functions, including the health of our nervous system. Understanding the connection between mitochondrial function, nervous system regulation, and aging can offer us powerful insights into how we can naturally reverse symptoms of fatigue and stress, leading to a more energized and balanced life.
Understanding Mitochondria and Their Role in Health
What Are Mitochondria?
Mitochondria are often called the "powerhouses" of the cell because they are responsible for generating adenosine triphosphate (ATP), the main energy currency of the cell. Every cell in your body relies on ATP to perform its functions, from muscle contraction to hormone production. But mitochondria do much more than produce energy. They are involved in regulating the metabolic rate, controlling apoptosis (programmed cell death), and synthesizing essential molecules like steroid hormones, which play a role in stress response and immune function.
The Impact of Aging on Mitochondria
As we age, mitochondrial function naturally declines. This decline is partly due to the accumulation of mutations in mitochondrial DNA (mtDNA), which is more vulnerable to damage than nuclear DNA. Mitochondria are located near the electron transport chain (ETC), where reactive oxygen species (ROS) are produced during ATP generation. Over time, the buildup of ROS can lead to oxidative stress, damaging mitochondrial DNA and impairing the mitochondria’s ability to produce energy efficiently.
This mitochondrial dysfunction is a significant factor in aging and has been linked to various chronic conditions, including neurodegenerative diseases like Alzheimer's and Parkinson's, cardiovascular diseases, and metabolic disorders such as type 2 diabetes. It also contributes to the age-related loss of muscle mass and strength (sarcopenia), which can severely affect mobility and quality of life.
ARTICLE CONTINUES BELOW
How Mitochondrial Dysfunction Affects Your Nervous System
The Connection Between Mitochondria and the Nervous System
Your nervous system, particularly your brain, is one of the most energy-demanding parts of your body. Neurons, the primary cells of the nervous system, require a constant supply of ATP to maintain their functions, including signal transmission and neuroplasticity (the ability of the brain to reorganize itself). When mitochondrial function is compromised, neurons struggle to produce enough energy, leading to impaired communication within the nervous system. This dysfunction can manifest as cognitive decline, mood disorders, and a decreased ability to manage stress—symptoms that many people experience as they age.
Nervous System Dysregulation: The Role of Stress and Mitochondria
Stress plays a crucial role in the health of your nervous system and is closely linked to mitochondrial function. The mitochondria are central to the body's response to stress because they regulate the production of ATP, which fuels the stress response, and control apoptosis, which determines whether a cell survives stress or undergoes programmed death.
When stress is chronic, it can overwhelm the mitochondria, leading to increased production of ROS and subsequent oxidative damage. This impairs mitochondrial function and exacerbates nervous system dysregulation, making it harder for your body to cope with stress. This vicious cycle can lead to symptoms like fatigue, anxiety, and depression, which are commonly associated with aging.
Stress, Mitochondrial Function, and Nervous System Dysregulation: A Deeper Dive
Stress is an inherent part of life, and our bodies are equipped with sophisticated mechanisms to manage it. The mitochondria, often known as the "powerhouses" of the cell, are integral to these mechanisms. Their role extends far beyond energy production—they are key players in the body’s stress response and the regulation of cell survival. Understanding this relationship is crucial, especially when considering how chronic stress can disrupt these processes, leading to significant health issues.
The Dual Role of Mitochondria in Stress Response
Mitochondria are responsible for producing ATP (adenosine triphosphate), which is vital for fueling the body's stress response. When you encounter stress, whether it's physical, emotional, or environmental, your body demands more energy to respond effectively. Mitochondria meet this demand by increasing ATP production, ensuring that your cells, especially those in the nervous system, have the energy required to function under pressure.
However, mitochondria are also involved in controlling apoptosis, the process of programmed cell death. This is a protective mechanism that removes damaged cells, preventing them from becoming dysfunctional or cancerous. During stress, cells that are too damaged to recover are typically targeted for apoptosis. Thus, mitochondria act as gatekeepers, deciding whether a cell will survive or be eliminated.
The Impact of Chronic Stress on Mitochondrial Function
While mitochondria are well-equipped to handle short bursts of stress, chronic stress presents a different challenge. When stress is prolonged, the constant demand for ATP significantly strains the mitochondria. This overactivity increases the production of reactive oxygen species (ROS), which are byproducts of ATP production.
In normal amounts, ROS play a role in cell signaling and defense against pathogens. However, ROS becomes harmful when produced in excess, as during chronic stress. They cause oxidative damage to mitochondrial DNA, proteins, and lipids, impairing the mitochondria's ability to function efficiently. This oxidative stress reduces ATP production and triggers more apoptosis, leading to a loss of healthy cells in tissues critical for maintaining homeostasis, such as the brain.
The Vicious Cycle of Mitochondrial Dysfunction and Nervous System Dysregulation
As mitochondrial function declines due to chronic stress, the nervous system begins to suffer. Neurons, the primary cells of the nervous system, have exceptionally high energy demands because they are constantly active—sending and receiving signals, maintaining synaptic function, and supporting cognitive processes. When dysfunctional mitochondria compromise their energy supply, their communication ability is diminished.
This leads to nervous system dysregulation, manifesting as symptoms like fatigue, anxiety, and depression. Fatigue occurs because cells do not produce enough ATP to meet the body's energy needs. Anxiety and depression can arise because the brain's neurotransmitter systems, which are heavily reliant on adequate mitochondrial function, become imbalanced. For instance, serotonin and dopamine, neurotransmitters that regulate mood and emotional well-being, require significant energy for their synthesis, release, and reuptake. When mitochondrial ATP production falters, these processes are disrupted, contributing to mood disorders.
Why This Matters as We Age
The implications of stress-induced mitochondrial dysfunction are particularly concerning as we age. As natural mitochondrial efficiency declines with age, adding the burden of chronic stress can accelerate the deterioration of both physical and mental health. Older adults may experience more pronounced symptoms of nervous system dysregulation, such as persistent fatigue, increased susceptibility to stress, and a higher risk of neurodegenerative diseases.
Furthermore, the body's ability to repair oxidative damage decreases with age, meaning that the ROS produced during chronic stress can cause more extensive harm. This creates a scenario where the aging nervous system is increasingly vulnerable to the detrimental effects of stress, making stress management and support of mitochondrial health critical components of healthy aging.
Lifestyle Factors That Cause Mitochondrial Dysfunction
1. Poor Diet | High in Processed Foods, Sugar, and Excessive Meat Consumption
One of the most significant contributors to mitochondrial dysfunction is diet, particularly one high in processed foods, refined sugars, and excessive meat consumption.
Processed Foods and Refined Sugars: These foods are typically low in nutrients and high in empty calories. Consuming large amounts of sugar can lead to insulin resistance, a condition where your cells become less responsive to insulin, leading to elevated blood sugar levels. High blood sugar increases the production of advanced glycation end-products (AGEs), which can damage proteins and lipids in the mitochondria, impairing their function. In fact, a study published in JAMA Internal Medicine found that diets high in added sugars are associated with a significantly increased risk of dying from cardiovascular disease, which is closely linked to mitochondrial dysfunction.
Excessive Meat Consumption: While protein is essential for health, diets overly rich in red and processed meats can contribute to oxidative stress and inflammation, both of which harm mitochondrial function. Meat, especially when cooked at high temperatures, can also produce harmful compounds like heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs), which further increase oxidative stress. Research published in The American Journal of Clinical Nutrition found that high consumption of red and processed meats is associated with a 20% increased risk of mortality, likely due to the oxidative stress and inflammation that these foods induce, which impairs mitochondrial function. However, we do not need meat to meet our protein requirements. In fact, studies have shown that plant-based proteins, such as those from legumes, nuts, seeds, and whole grains, are not only sufficient to meet dietary needs but also offer additional benefits by being lower in saturated fats and free from harmful compounds like HCAs and PAHs. Moreover, plant-based diets have been associated with reduced inflammation and improved mitochondrial efficiency.
2. Sedentary Lifestyle | A Major Contributor to Mitochondrial Dysfunction
A sedentary lifestyle significantly contributes to mitochondrial dysfunction, as regular physical activity is essential for maintaining mitochondrial efficiency and stimulating mitochondrial biogenesis. When you don’t engage in sufficient exercise, your mitochondria become less effective at producing ATP, the energy currency of cells. Over time, this inefficiency can lead to a decrease in both the quantity and function of mitochondria, leaving you feeling fatigued and with lower energy levels. According to the World Health Organization (WHO), insufficient physical activity contributes to approximately 3.2 million deaths annually, underscoring the global impact of sedentary behavior on health.
Lack of Physical Activity: Physical inactivity directly reduces the efficiency of mitochondria. Regular exercise activates enzymes involved in oxidative phosphorylation, the process that generates ATP. Without this stimulation, mitochondrial activity declines, leading to reduced energy production and increased fatigue. A study published in The Journal of Clinical Investigation found that sedentary individuals had significantly lower mitochondrial content and activity, associated with higher levels of inflammation and an increased risk of metabolic syndrome.
Muscle Atrophy: Sedentariness also leads to muscle atrophy, or the loss of muscle mass, which is closely linked to reduced mitochondrial density. Muscles are highly metabolically active tissues that house a large number of mitochondria. When muscle mass decreases due to inactivity, the number of mitochondria also declines, diminishing the body's overall capacity to produce energy. Research published in The American Journal of Physiology shows that even short periods of inactivity can cause significant muscle atrophy and a corresponding decline in mitochondrial content, leading to overall tiredness and weakness.
3. Chronic Stress and Poor Sleep
Chronic stress is another major contributor to mitochondrial dysfunction. When you are constantly stressed, your body is in a heightened state of alert, requiring more ATP to fuel the stress response. As mentioned earlier, this increased demand leads to the overproduction of ROS, which damages mitochondria.
Chronic Stress: Chronic stress significantly impairs mitochondrial function by increasing the production of reactive oxygen species (ROS) and reducing ATP production efficiency. A study in Psychoneuroendocrinology found that prolonged exposure to stress hormones like cortisol leads to mitochondrial dysfunction, contributing to cellular aging and a diminished ability to manage stress. This stress-induced oxidative stress damages mitochondrial DNA, further impairing energy generation. According to the American Psychological Association (APA), about 75% of Americans report experiencing stress symptoms such as headaches, fatigue, or sleep disturbances, which are linked to an increased risk of mental health disorders, cardiovascular disease, and metabolic syndrome—all associated with mitochondrial dysfunction.
Poor Sleep: Sleep is crucial for repairing and maintaining mitochondrial function. A study published in Sleep found that sleep deprivation significantly decreases mitochondrial activity and increases oxidative stress in the brain, leading to cognitive decline and mood disturbances. Poor sleep quality impairs the body's ability to repair damaged mitochondria, resulting in accumulated cellular damage and a higher risk of neurodegenerative diseases. According to the CDC, one in three adults in the U.S. does not get enough sleep, which is associated with a 48% increased risk of heart disease and a 15% increased risk of stroke, highlighting the essential role of sleep in maintaining mitochondrial health and overall well-being.
4. Environmental Toxins and Pollutants
We are constantly exposed to various environmental toxins, which can accumulate in our bodies over time and significantly impact mitochondrial function.
Air Pollution and Heavy Metals: Exposure to pollutants like air pollution, pesticides, and heavy metals (such as mercury and lead) can lead to oxidative stress, directly damaging mitochondria. These toxins can disrupt mitochondrial membranes, impair ATP production, and increase the risk of chronic diseases.
Household Chemicals: Even household cleaning products and personal care items can contain harmful chemicals contributing to oxidative stress. Long-term exposure to these toxins can impair mitochondrial function and increase the likelihood of experiencing fatigue and other health issues.
5. Excessive Use of Technology and Social Media Scrolling
While technology is a powerful tool, excessive social media use can negatively affect mitochondrial health.
Mental Overstimulation: Constantly scrolling through social media feeds can lead to mental overstimulation, which activates the body's stress response. When you're engaged in this kind of overstimulation, your brain is bombarded with a rapid stream of information, often accompanied by emotional highs and lows from what you read and see. This triggers the release of stress hormones like cortisol, which increases the demand on your mitochondria to produce ATP to fuel the stress response. Over time, this chronic demand for energy leads to mitochondrial overwork, contributing to mental fatigue and increasing oxidative stress within the brain. A survey by the Pew Research Center found that 64% of American adults say social media has a mostly negative effect on their mental health, often citing stress and anxiety as primary concerns. This persistent stress from digital overload can lead to a decline in mitochondrial efficiency and overall cognitive function.
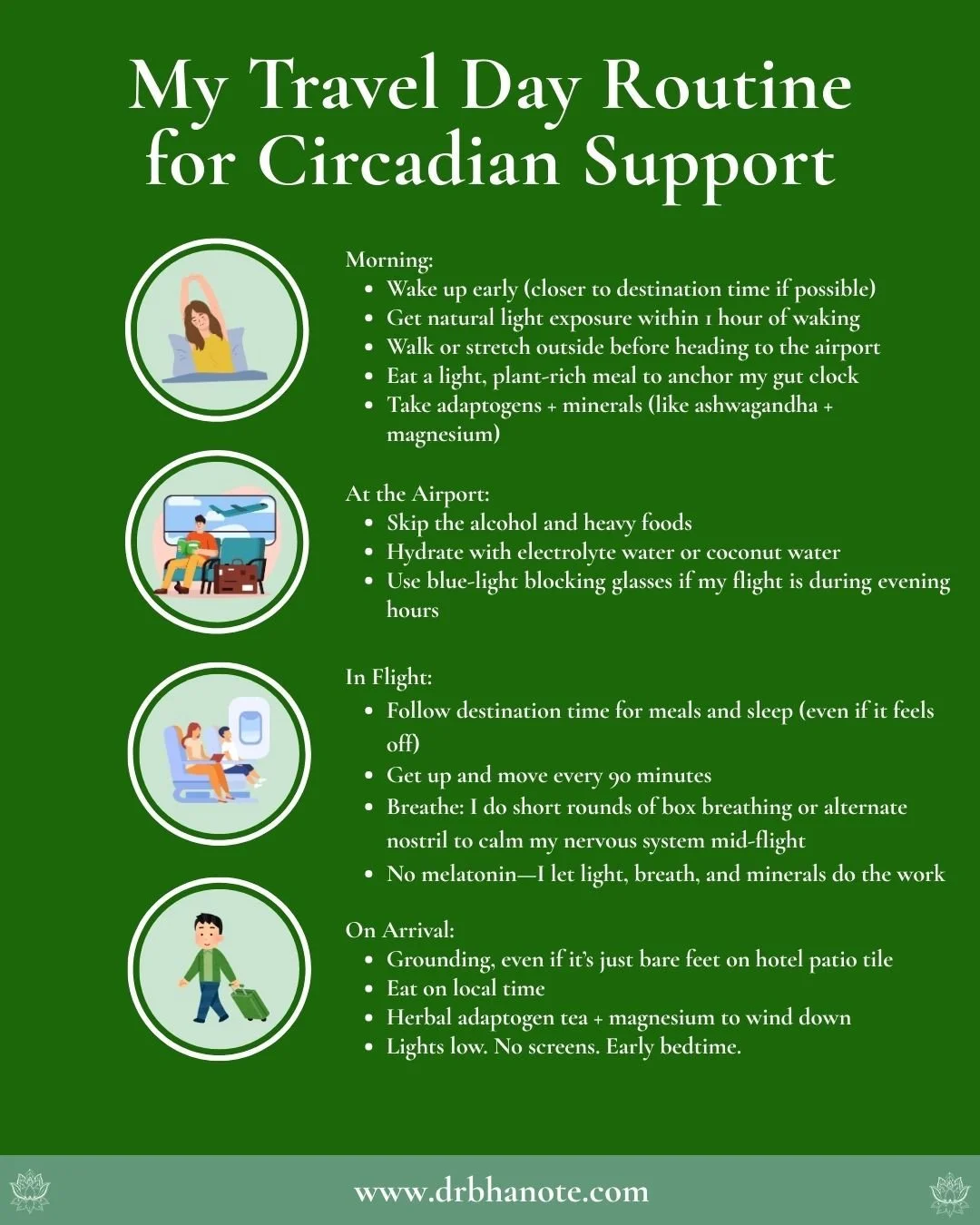
Blue Light Exposure: Another significant concern is the prolonged exposure to blue light emitted by screens, which can disrupt your circadian rhythm and negatively impact sleep quality. Blue light, especially during evening hours, interferes with melatonin production, the hormone responsible for regulating sleep. Disrupted sleep patterns prevent your mitochondria from undergoing necessary repair processes, leading to accumulated damage and decreased mitochondrial function. According to the National Sleep Foundation, 90% of Americans report using an electronic device within an hour of going to bed, a habit strongly linked to poorer sleep quality and increased risk of sleep disorders. This disruption not only affects your overall health but also specifically impairs mitochondrial regeneration, which is critical for maintaining energy levels and preventing age-related diseases.
6. Smoking and Excessive Alcohol Consumption
Both smoking and excessive alcohol consumption are well-known to contribute to oxidative stress and inflammation, which are harmful to mitochondria.
Smoking: The chemicals in cigarette smoke generate a large number of free radicals, which can cause severe oxidative damage to mitochondrial DNA and impair their function.
Alcohol: Excessive alcohol consumption disrupts metabolic processes and increases the production of ROS. Over time, this can lead to mitochondrial damage, particularly in the liver, which is central to detoxifying the body.
The Consequences of Mitochondrial Dysfunction
When these lifestyle factors combine, they create a perfect storm for mitochondrial dysfunction. The consequences are far-reaching:
Accelerated Aging: Mitochondria are integral to the aging process. Dysfunctional mitochondria lead to decreased energy production, increased oxidative stress, and cellular damage, all of which contribute to accelerated aging. This can manifest as premature wrinkles, decreased muscle mass, cognitive decline, and a general feeling of being "worn out."
Fatigue: With impaired mitochondria, your cells struggle to produce the energy they need, leading to persistent feelings of fatigue and a lack of vitality, regardless of how much rest you get.
Increased Risk of Chronic Diseases: Mitochondrial dysfunction is linked to a range of chronic diseases, including neurodegenerative diseases (like Alzheimer’s and Parkinson’s), cardiovascular diseases, diabetes, and even certain cancers. Failing to address the lifestyle factors that harm mitochondria increases your risk of developing these conditions.
Mental Health Issues: As mitochondrial function declines, so does the brain’s ability to regulate mood and cognition. This can lead to symptoms of depression, anxiety, brain fog, and cognitive decline.
Recognizing the lifestyle factors contributing to mitochondrial dysfunction is the first step toward improving your energy levels, slowing aging, and enhancing overall health. By understanding how diet, physical activity, stress, environmental toxins, and technology use impact your mitochondria, you can make informed choices that protect these vital organelles and promote long-term wellbeing. The good news is that many of these factors are within your control, and by making positive changes, you can support your mitochondria and feel more energized, focused, and resilient as you age.
Practical Steps to Rejuvenate Mitochondria and Regulate the Nervous System
How Exercise Promotes Mitochondrial Health
Exercise is one of the most effective ways to improve mitochondrial function and, by extension, support nervous system health. Physical activity stimulates mitochondrial biogenesis, the process of creating new mitochondria within cells. This process is regulated by several key signaling pathways, including the peroxisome proliferator-activated receptor-gamma coactivator 1-alpha (PGC-1α), often referred to as the "master regulator" of mitochondrial biogenesis.
When you engage in exercise, particularly endurance and high-intensity interval training (HIIT), PGC-1α is activated, increasing mitochondria’s number and efficiency. This results in greater ATP production, better management of oxidative stress, and improved overall cellular health.
Exercise and the Nervous System: Enhancing Stress Resilience
Exercise also profoundly affects the nervous system, particularly in enhancing stress resilience. Physical activity increases the production of brain-derived neurotrophic factor (BDNF), a protein that supports the survival and growth of neurons. BDNF not only improves mitochondrial function in neurons but also promotes neuroplasticity, which is crucial for maintaining cognitive function and emotional stability as we age.
In addition, regular exercise helps regulate the hypothalamic-pituitary-adrenal (HPA) axis, the central stress response system in the body. By promoting a balanced release of cortisol—the primary stress hormone—exercise can reduce the impact of chronic stress on both the mitochondria and the nervous system, leading to better stress management and improved overall wellbeing.
Incorporating the Right Types of Exercise
To optimize mitochondrial health and nervous system regulation, it’s essential to incorporate a variety of physical activities into your routine:
Endurance Exercise: Activities such as running, cycling, and swimming are excellent for promoting mitochondrial biogenesis and enhancing aerobic capacity. Aim for at least 150 minutes of moderate-intensity endurance exercise per week.
High-Intensity Interval Training (HIIT): HIIT involves short bursts of intense exercise followed by periods of rest or low-intensity activity. This type of training is particularly effective in stimulating mitochondrial biogenesis and improving metabolic flexibility. Incorporate HIIT sessions into your routine 2-3 times per week.
Resistance Training: Strength training exercises, such as weightlifting or bodyweight exercises, help maintain muscle mass and mitochondrial function, especially in older adults. Aim for at least two resistance training sessions per week.
Flexibility and Balance Exercises: Incorporating activities like yoga or Pilates can help improve flexibility, balance, and nervous system regulation, further supporting mitochondrial health.
Supporting Mitochondrial Function with Nutrition and Lifestyle
Exercise is crucial, but it’s equally important to support your mitochondria and nervous system with the proper nutrition and lifestyle choices:
Nutrient-Dense Diet: A diet rich in antioxidants—such as those found in fruits, vegetables, nuts, and seeds—can help protect mitochondria from oxidative stress. Foods high in B vitamins, magnesium, and coenzyme Q10 are also essential for supporting mitochondrial function.
Intermittent Fasting: Intermittent fasting has been shown to promote mitochondrial biogenesis and enhance metabolic flexibility. Consider incorporating intermittent fasting protocols, such as time-restricted eating, into your routine to support mitochondrial health.
Stress Management: Chronic stress impairs mitochondrial function, so it’s essential to incorporate stress management techniques such as mindfulness meditation, deep breathing exercises, and adequate sleep into your lifestyle.
Hydration: Adequate hydration is vital for maintaining cellular function, including that of mitochondria. Ensure you are drinking enough water throughout the day to support overall health.
Regulate Your Nervous System and Thrive Through Community
As we age, it’s easy to feel that fatigue, stress, and diminished vitality are inevitable. But by understanding the vital role that mitochondria and nervous system regulation play in our overall health, we can take proactive steps to age gracefully and energetically. The path to rejuvenating your energy and resilience lies in making intentional lifestyle changes—choices that support your mitochondria and regulate your nervous system.
These changes are not just about diet and exercise; they’re about embracing a holistic approach to wellbeing. Consider integrating the powerful rituals from The Anatomy of Wellbeing, which guide you through practices designed to enhance your mitochondrial function and overall vitality. Join me at one of our Longevity Retreats, where we focus on these principles in an immersive, in-person experience, or connect with our community inside the Lifestyle Design Lab. Here, regulating the nervous system through mindful living is our priority, helping you to not just live longer, but to live better.
Remember, every small, intentional step you take—whether it's adjusting your diet, engaging in regular physical activity, or practicing stress management—brings you closer to a life filled with energy, purpose, and joy. Start today, and discover the power of living well, not just in years, but in the quality and vibrancy of each moment.
MAKE A DIFFERENCE BY SHARING THIS ARTICLE WITH OTHERS TO ENCOURAGE WELLBEING ⤵
References:
Yang, Q., Zhang, Z., Gregg, E. W., Flanders, W. D., Merritt, R., & Hu, F. B. (2014). Added Sugar Intake and Cardiovascular Diseases Mortality Among US Adults. JAMA Internal Medicine, 174(4), 516–524.
Larsson, S. C., & Orsini, N. (2014). Red Meat and Processed Meat Consumption and All-Cause Mortality: A Meta-Analysis. The American Journal of Clinical Nutrition, 99(3), 726–737.
Petersen, K. F., & Shulman, G. I. (2002). Pathogenesis of Skeletal Muscle Insulin Resistance in Type 2 Diabetes Mellitus. The Journal of Clinical Investigation, 106(1), 3-7.
Booth, F. W., & Laye, M. J. (2010). The Decline in Skeletal Muscle Mitochondrial Content with Age and its Association with Insulin Resistance and Type 2 Diabetes. The American Journal of Physiology - Endocrinology and Metabolism, 296(6), E1134-E1140.
Lee, I. M., & Shiroma, E. J. (2012). Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. The Lancet, 380(9838), 219-229.
Wallace, D. C. (2012). Mitochondria and Cancer. Cell Metabolism, 16(5), 671-680.
The information on this website has not been evaluated by the Food & Drug Administration or any other medical body. We do not aim to diagnose, treat, cure or prevent any illness or disease. Information is shared for educational purposes only. You must consult your doctor before acting on any content on this website, especially if you are pregnant, nursing, taking medication, or have a medical condition. Our content may include products that have been independently chosen and recommended by Dr. Monisha Bhanote and our editors. We may earn a small commission if you purchase something mentioned in this article.
YOU MAY ALSO LIKE:
by Dr. Monisha Bhanote
✅ EVIDENCE-INFORMED REVIEWED ARTICLE